Facts
All kinds of cancer, including childhood cancer, have a common disease process. Cells grow out of control, develop abnormal sizes and shapes, ignore their typical boundaries inside the body, destroy their neighbor cells, and ultimately can spread (or metastasize) to other organs and tissues. As cancer cells grow, they demand more and more of the body's nutrition. Cancer takes a child's strength, destroys organs and bones, and weakens the body's defenses against other illnesses.
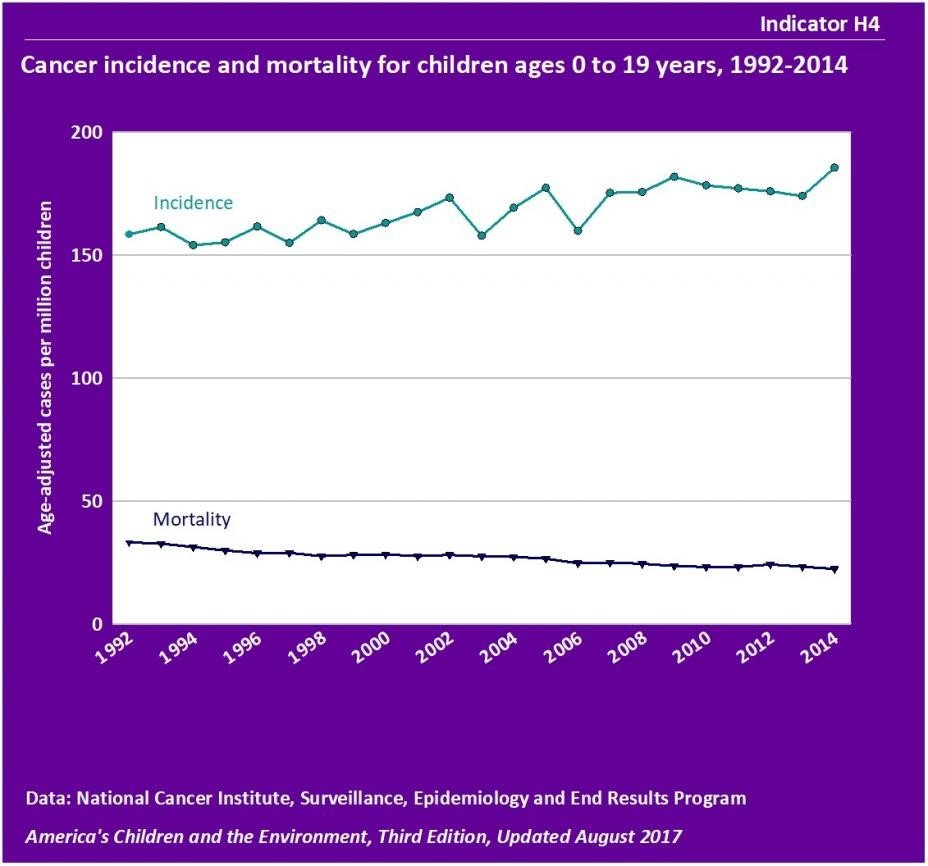
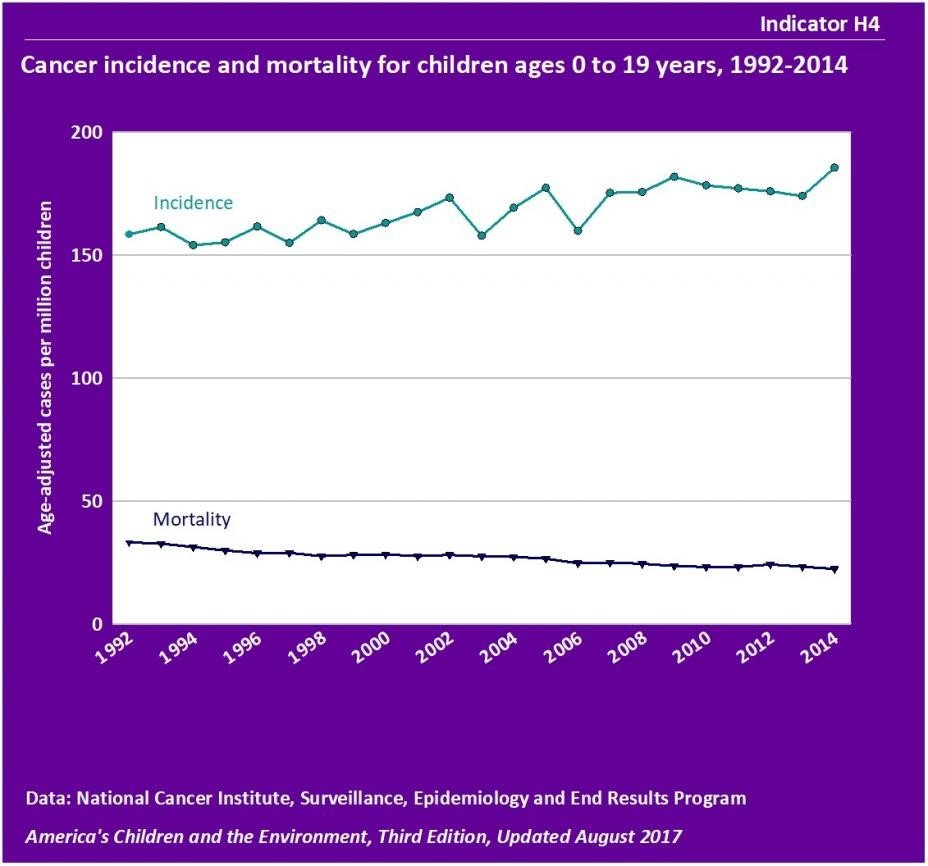
The burden of cancer among our nation's children has been increasing slightly, by about 0.6% per year, since 1975. Cancer related mortality in children ages 0-14 has been decreasing by 0.9% per year since 1997. The 5-year relative survival rate for all three age groups has increased significantly since the mid 1970s. For example, among children ages 10-14 years, the 5-year relative survival rate increased from 58.9% for those diagnosed in 1975-77 to 80.8% for those patients diagnosed in 1999-2005.
Cancer Statistics


Cancer is a complex disease that involves over 100 different variations or subtypes. While 99% of cancer develops in adults, 1 in every 285 children will have cancer before they reach the age of 20. For those children that are diagnosed with the disease, there is confusion and pain, and a litany of treatments that drag the entire family into overwhelming turbulence.
The most horrifying words parents can hear is “your child has cancer.” We have put together some of the basic information and statistics to assist in trying to make order out of the chaos of cancer. The information has been gathered from various reliable sources that study and report on cancer and may be one or more years old based on the report results.
What is Childhood Cancer?
Cancer in children can happen anywhere within their bodies and can include the lymph node systems, the blood, the central nervous system (brain and spinal cord), kidneys, liver, pancreas, and other tissues and organs. Science doesn’t know the cause for childhood cancers. Even when the cancer in children starts in the same part of the body, they can behave differently than cancer in adults.
The disease of cancer starts when what once were normal healthy cells begin to grow and reproduce out of control. In a majority of these types of cancer they form a tumor. Benign tumors can form which are non-cancerous, but it is the malignant tumors that are the cancer agents that then spread throughout the body if untreated.
Leukemia is a type of cancer that begins in the bone marrow and rarely forms a solid tumor. Leukemia cancer cells push out other types of healthy cells in the bone marrow and that prevents the production of:
- The white blood cells that are used by the body to fight infection.
- The normal red blood cells that carry oxygen to the tissues in the body.
- The platelets which are required for the clotting of blood.
Types of Childhood cancer:
Childhood cancer describes a range of cancer types that attack children and is also called pediatric cancer.
Leukemia accounts for nearing 29% of cases of childhood cancer for children 0-14 years old; while the balance of nearing 50% of childhood cancer diagnosis also includes brain and central nervous system tumors and lymphomas, and sarcomas. In kids 15-19 years of age, the most common types of cancer are brain and other CNS (central nervous system) lymphomas and tumors, which are followed by leukemia, ovarian and testicular (gonadal) germ cell tumors, thyroid cancer, and melanoma; with numerous additional types of childhood cancer.
How many children are diagnosed with cancer in the U.S. annually?
The estimation in 2017 listed 15,270 children and adolescents from ages of 0-19 were diagnosed with cancer and 1,790 of these children died of the disease.(1) Compare this to the 2007 statistic of around 10,400 U.S. children under 15 years of age diagnosed with cancer and 1,545 deaths from the disease. (2) While the numbers of diagnosed have increased, the number of deaths have decreased from 15% to 12%.
What are the changes in survival rates for childhood cancer?
In the 1970’s, the five-year survival rate for children diagnosed with cancer was around 58%. While we have seen incredible advances in the last number of decades, the current five-year survival rate is nearing 80% of children with cancer. The statistics are complex because as survival rate depends on cancer types and other factors. (2)
The treatments that were introduced in the 1960s and 1970s increased the five-year survival rate for children diagnosed with:
- Acute lymphoblastic leukemia at ages 0-14 years from 57% in 1975 to 92% in 2012.
- Non-Hodgkin lymphoma at ages 0-14 years from 43% in 1975 to 91% in 2012. (3)
The change in survival rates has also altered the statistics so that brain cancer has replaced leukemia as the leading cause of cancer death among children. (4)
The mortality rate of cancer per 100,000 people in a year has declined. Among children and adolescents covering ages 0-19 years, the reduction has been over 50% from 1975-2015. (5) The mortality rate in children and adolescents in 1975 was 5.1 per 100,000 individuals and 2.3 per 100,000 children and adolescents in 2015.
Between 1999 and 2014, the rate of death due to cancer reduced the most for children ages 1-4 (26% drop), followed by a 22% reduction for 15-19 year-olds, a 19% reduction for 10-14 year-olds, and a 14% drop for 5-9 year-olds. (6)
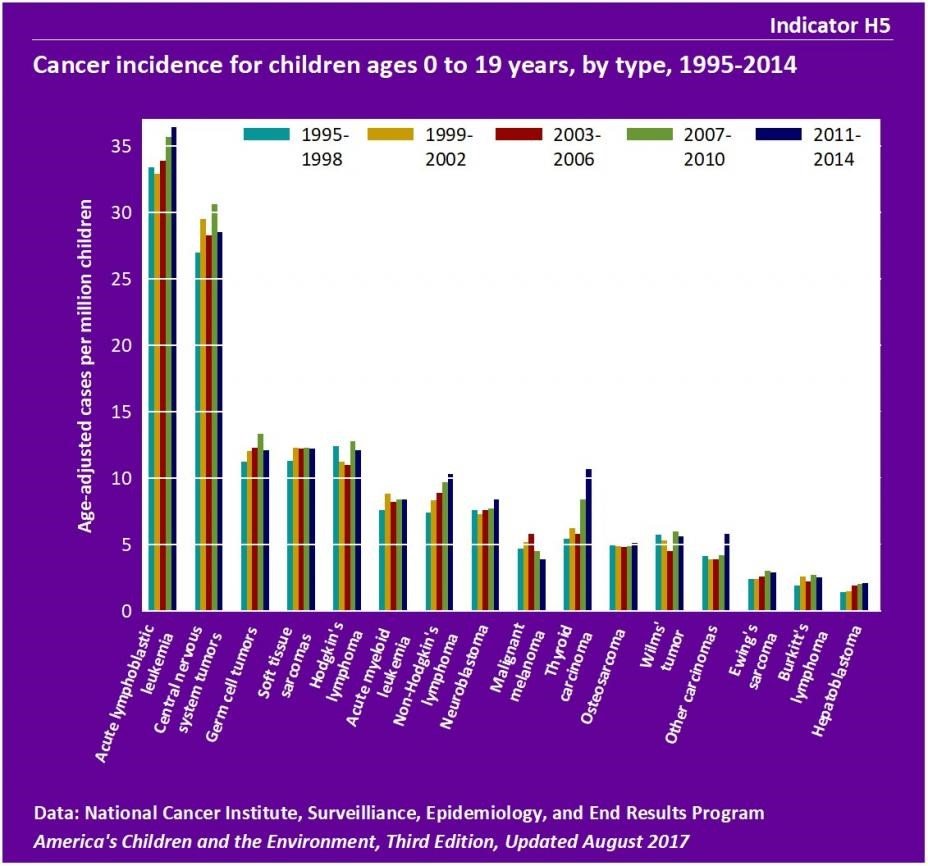
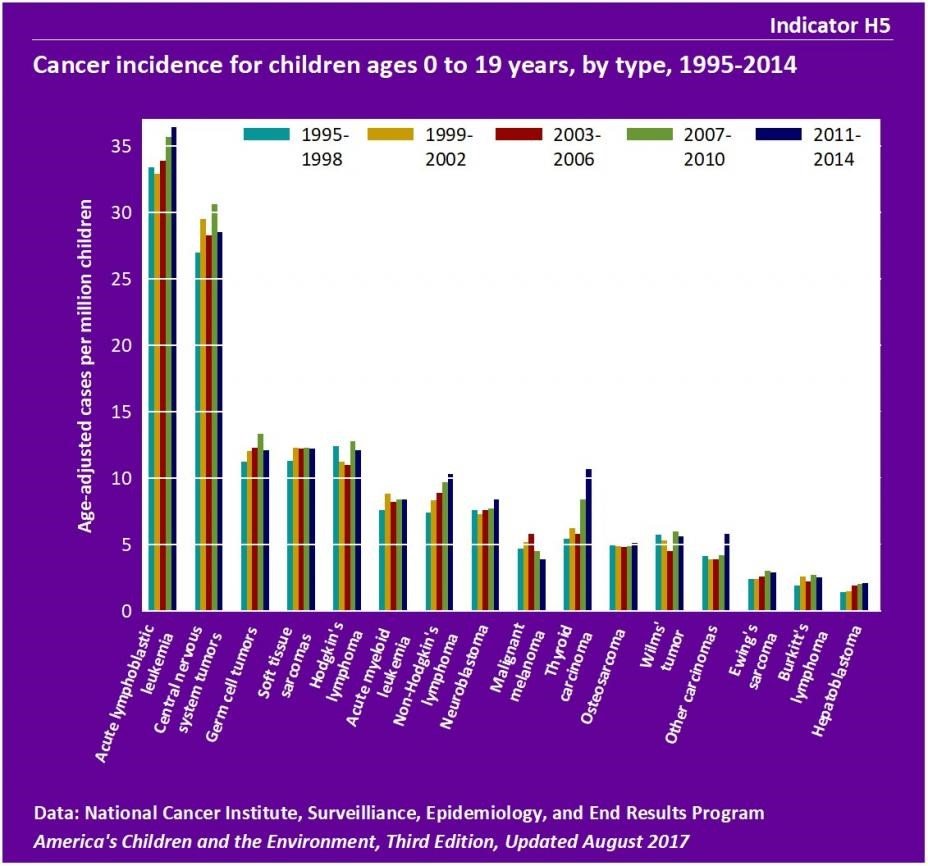
Between the years of 2011-2014, lymphomas, which include Hodgkin's lymphoma, non-Hodgkin's lymphoma, and Burkitt's lymphoma, represented 14% of childhood cancers. Incidence of Hodgkin's lymphoma was 12.4 cases per million in 1995-1998 and 12.1 per million in 2011-2014. There were approximately 7 cases of non-Hodgkin's lymphoma per million children in 1995-1998 and 10 per million in 2011-2014. Incidence of Burkitt's lymphoma was 1.9 cases per million children in 1995-1998 and 2.5 per million in 2011-2014. (7)
Even with the advances in technologies and treatments, it is clear that additional research must continue.
The breakdown of years, age, gender, and ethnicity of the various childhood cancer data can be found in more detail in the childhood cancer incidents and mortality report epa.gov report.
Some of the new technologies developed in the 1980s for detection included the MRI (magnetic resonance imaging) that allowed a visual image of brain tumors that couldn’t be easily seen with older equipment types. It is believed that the more widespread use of such technologies as MRIs increased earlier detection. There was also a reclassification of some brain tumors that were listed as “benign” to be changed to “malignant,” as well as improvements in neurosurgical techniques for biopsies of brain tumors.
What are the known and suspected causes of childhood cancer? +" collapse_text="What are the known and suspected causes of childhood cancer?
When a family is given a diagnosis of cancer in their child the very first question is “why?” While science continues research to try to address this question, the answers are very complex and some are still yet unknown.
Risk factors involve a complicated list to examine including such topics as genetics, environment, lifestyle, and overall health conditions. Yet even these don’t address all of the nuances involved in the development of cancer in children; they are simply a starting point. A risk factor is anything that could increase an individual’s chance of development cancer. It’s important to note that most risk factors can “influence” the appearance of cancer but most are not the direct cancer cause. Each person is incredibly unique and while some may have quite a few risk factors and not develop cancer; others may not have any risk factors and they do develop cancer.
Researchers don’t have a single answer for the causes of most of the childhood cancers. There are a very small percentage of cancers that share a link with the Down syndrome genetic disorder and others are genetic abnormalities that are inherited as well as radiation treatments.
Around 10% of all childhood cancers are caused by what is called “germline mutation.” This is a gene mutation that can be passed from parents to their children. Around 45% of children with a cancer of the eye that develops mostly in children known as “retinoblastoma” is inherited as a gene mutation in the RB1 gene from a parent. (8). Other inherited mutations that are linked with certain syndromes that are family-related include: Li-Fraumeni syndrome, Beckwith-Wiedemann syndrome, Fanconi anemia syndrome, Noonan syndrome, and von Hippel-Lindau syndrome. (9)
To assist doctors and scientists to learn additional information about risk factors, a childhood cancer registry has been created by the Children’s Oncology Group (COG). Once a child is registered in the network, families and patients may be contacted by researchers and doctors to collect information for the studies on environmental and genetic factors that may lead to a connection to childhood cancer development.
While exposure to toxic and infectious substances are unlikely to be the root cause of cancer in children, there are some that have been linked to childhood cancer. These include ionizing radiation which can lead to leukemia development and other childhood and adolescent cancers. Children that had mothers that were exposed to x-rays during pregnancy as well as children that had after birth CTI after birth diagnostic medical radiation scans have also been shown to have an increase in brain tumors, leukemia, and potentially other cancers. (10)
Ongoing studies have more recently shown that there are possible links to childhood cancer with additional environmental exposures to such things as certain pesticides used around and in the home, some solvents found in household products, and air pollution. Additional research may have identified a few factors that reduce the risk of cancer in children. These have included folate consumption by the mother during pregnancy that has been associated with the reduction in risk of both brain tumors and leukemia in children, being breastfed, and exposure to routine childhood infections that are also associated with reduced childhood leukemia risks. (11)(12)
The difference between pediatric and teenage cancer patients
Those children that are teenagers, ages 15-19, are beginning to enter young adulthood and have unique social, emotional, and medical needs from those of younger children. This group of children have types of cancer that are most commonly found in adults including:
- Hodgkin lymphoma (15%) and Non-Hodgkin lymphoma (8%)
- Germ cell tumors, including testicular cancer (8%) and ovarian cancer (2%)
- Central nervous system (CNS) tumors (10%)
- Thyroid cancer (11%)
- Melanoma (6%)
- Acute lymphoblastic leukemia (ALL) (8%)
- Soft tissue sarcoma (7%)
- Bone tumors (7%) including osteosarcoma and Ewing sarcoma
- AML (4%)
What research is being done for childhood cancer?
More research is needed as well as developing new, more effective and safer childhood cancer treatments. Even with long-term survival, many childhood cancer survivors may experience life-long adverse effects from the treatments of the disease.
For children and adolescents, cancer is the leading cause of death from disease. National Cancer Institute (NCI) has a number of programs in place that are focused on childhood cancers, and other programs that are applicable to cancer in children. NIH supports a range of biomedical research that relates to childhood cancer including:
• Basic research to enhance our understanding of the fundamental mechanisms of cancer
• Clinical research to test new treatments for safety and effectiveness
• Survivorship research to reduce the long-term adverse effects of cancer and its treatment
Challenges:
The challenges that are presented with childhood and adolescent cancer include that fact that they are relatively uncommon. Since they represent only 1% of all newly diagnosed cancers in the U.S. every year, the number of children that are patients are small. This situation creates a dichotomy for the various institutions to address the complex biological questions and requires collaboration among all of the researchers.
Clinical trials for the science of cancer in children are restricted to small patient numbers that are defined by the tumor molecular characteristics instead of the location of origin of the tumors in their bodies. Collaboration among all clinical research organizations is continuing so that it creates trials with sufficient numbers of patients so that they can have meaningful results that can be of benefit. This requires more efficient methods to curate and share research that is gathered including data from genomic studies to clinical outcomes.
One of the greatest challenges in childhood cancer research is that the causes of these cancers are unknown. Unlike cancer in adults that can sometimes be attributed to specific risk factors, it is difficult to identify causes. The types of cancers that develop in children also differ from those in adults, attacking organs. This makes the development of drug therapies difficult, as adult cancer drug therapies are created to target signaling pathways and these are required pathways in children for normal development.
Promising New Developments

References
(1) www.cancer.gov/about-cancer/understanding/statistics
(2) www.cancer.org/cancer/cancer-in-children/key-statistics
(3) Jemal A, Ward EM, Johnson CJ, et al. Annual Report to the Nation on the status of cancer, 1975-2014, featuring Survival. Journal of the National Cancer Institute 2017; 109(9). [PubMed Abstract]
(4) www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
(5) www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
(6) www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
(7) www.epa.gov/ace/ace-health-childhood-cancer
(8) www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
(9) www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
(10) www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
(11) www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
(12) www.cancer.gov/types/childhood-cancers/child-adolescent-cancers-fact-sheet
Could This Be Cancer?
Cancer is complicated. While most of the signs we notice turn out to be something that isn’t serious, there are several you should keep an eye out for.
What Is Leukemia?
Leukemia is usually thought of as a children’s condition, but it actually affects more adults. It’s more common in men than women, and more in whites than African-Americans.
Facts
- Among children ages 0-14, cancer causes more deaths in the U.S. than any other disease.
- Childhood cancer kills over 1600 children every year.